Week Zero: days 0-6
Around 40 weeks after conception, your baby has outgrown the available space inside the womb and relocated to the outside world! Pregnancy and birth retreat to the past as your whole focus becomes a week of firsts for this new person in your life.
From the vital first hour and the first breastfeed to the first nappy of around 2000 changes in the first year alone - strap on those training wheels as there is a steep learning curve ahead of you all!
The First Feeds
Whether your baby navigated their own way during The Magical Hour or needed a helping hand to attach, that first breastfeed is about much more than food. Your colostrum, the highly concentrated milk produced in pregnancy and the early days after birth, is packed not only with nutrition but important bacteria to seed the infant gut. Referred to as the microbiome, what you might know as gut flora is important for your baby’s digestion and immune system. Alongside the good bacteria collected during birth (through contact with the mother’s skin) this is the beginning of the gut population which will remain active throughout your child’s life.
Colostrum
Colostrum is the very first milk your body produces, typically beginning around 16 weeks gestation. While some mothers can express a few drops early on, and others find their breasts leaking in pregnancy, some might only notice a little dried colostrum on their nipple and many see none at all before their baby is born: all normal variations and not indicators of milk production or breastfeeding capability.
In recent years, expressing colostrum in late pregnancy and freezing it has become popular. While generally only advised for known risks of baby needing supplementary feeds in the first few days (eg: babies born to mothers with gestational diabetes), many people choose to store colostrum "just in case". Sometimes circumstances of birth or immediate postnatal period compromise the establishment of feeding at the breast and supplementation might be medically recommended. In those circumstances, the concentrated colostrum you have collected and brought with you to the hospital can be used instead of infant formula. This should be done alongside efforts to improve milk removal from the breast by the baby and/or expressing to support breastmilk production.
In some cultures, colostrum has been seen very differently. While modern science has shown valuable nutrients and immune system support, colostrum was seen as unclean or unsafe by some. It is important to support babies to have this first food as nature intended. While respecting the beliefs of community elders, mothers need support to meet the current recommendations for babies to be exclusively breastfed from birth, without other food or drinks, unless medically required. This may or may not include traditional or ceremonial first foods.
Colostrum is packed with the nutrients babies need before the traditional milk "comes in", several days after birth and gives the infant gut important bacteria to support healthy digestion and immune protection.
Transitional Milk
You might be surprised to learn there is a stage between colostrum and mature breastmilk. Around 3-4 days, your body begins production of your mature breastmilk which mixes with the colostrum in the breast and together they become what we call transitional milk. This powerful cocktail retains all the benefits of colostrum, with an increase in the fluid and nutrients your baby needs. By around two weeks, your milk will be recognisable as what we think of as breastmilk.
Transitional milk can still look quite yellow and creamy. Frequent and effective removal of this milk - by the baby and/or by expressing - is important in establishing milk production. This can be one of the most challenging periods in breastfeeding as your baby will increase demand and seem constantly hungry despite frequent feeding. It is hard to believe that this is a normal part of establishing breastfeeding but your baby is working hard at programming your breasts to meet his needs and it is a demanding time for both of you. Sometimes this intense feeding period combined with your baby still working on getting attachment right can lead to sore or even cracked nipples. And all at the same time that hormonal changes in the mother brings on what is sometimes known as “the baby blues”. Not to be confused with postnatal depression, this mother of all mood swings can have you in tears over a lukewarm cup of tea and furious because your partner forgot to bring you clean pajamas. Combined with disrupted sleep and an increasingly wakeful baby, its a recipe for crisis.
The natural cycle of rapid breast filling and rapid breast emptying can sometimes get out of sync, leading to over-full, engorged breasts. The banked up breastmilk can also reduce the circulation of other fluids in and around the breast tissue, leading to swelling and discomfort. Engorgement can be prevented or minimised by frequent and effective removal of milk by the baby. Babies can feed ineffectively due to jaundice, issues like tongue tie or poor attachment. Expressing gently by hand or pump before feeding can help your baby take a wider mouthful of breast, while expressing after feeds receives the breast and reduces fullness. Removal of milk signals the breast to keep up production but full breasts can send the wrong message and reduce supply. You might even need to empty the breast as much as possible by expressing to get everything back on track.
It is around this stage that many new parents take their baby home from hospital. Often armed with instructions to “top up” the baby after each feed with expressed breastmilk (EBM) and/or infant formula and to express their milk by pump after every feed. Sometimes this is known as Triple Feeding. It can also be described as The Top-up Trap.
The most common reason for this situation is newborn weight loss.
Another cause is lack of sleep in mother and infant due to frequent feeding around the clock.
It is important to understand how both of these factors are not always cause for concern and, with the right response, are short-term consequences of the baby and breasts changing gears as they move to the next stage.
Understanding infant weight loss in the first week.
A newborn baby will nearly always lose weight in the first week of life. Most of this is fluid loss as they adapt from life immersed in amniotic fluid in the uterus. One reason a newborn is given at least two ID bands in hospital is invariably one will fall off as they lose this excess fluid gained naturally in the womb.
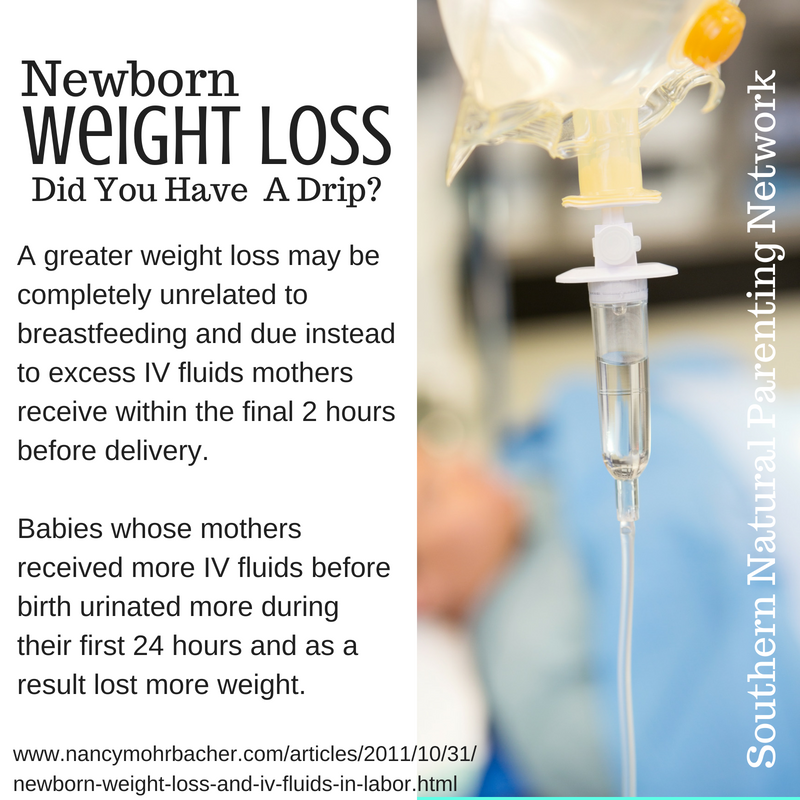
However, modern childbirth management has introduced additional fluid into the systems of many babies. Connecting women to an IV drip of saline is routine for all births in some parts of the world and is part of all caesarean births and most long and protracted labours and complicated deliveries. The fluid keeps mothers hydrated and allows drugs to be easily administered as needed. But while the baby and mother remain connected via the placenta, whatever fluid is added to the maternal bloodstream also ends up in the baby’s. Put simply, the baby at delivery may be retaining extra fluid, which is included in any weight recorded soon after birth. And when that weight in shed in addition to the normal newborn weight loss - an amount beyond the acceptable level might cause concern.
Some hospital protocols still require babies to be weighed before going to the breast for the first feed. Where the first hour is recognised and supported for its importance in establishing breastfeeding, weighing might be delayed for several hours or even to the following day. A discharge weight is also recorded before leaving hospital, which is usually before breastmilk has become transitional - or as many describe it - “come in”. The difference between the two measurements is calculated and a percentage of weight loss recorded. Anything higher than 10% is flagged as an indicator the baby may not be getting “enough” milk and supplementation recommended.
The days following hospital discharge are often the most vulnerable for breastfeeding. So much so, we are going to look at them in detail in Breastfeeding in the first 14 days.