Do you have a low milk supply?
Many people expect a breastfeeding mother to lose her milk. They believe milk supply can dry up suddenly. It is a case of when, not if, that a mother will need to begin supplementing with formula. In fact, some family, friends or even health professionals have so little faith in breastfeeding being successful, they suggest parents keep formula on hand at home, just in case.
Humans and other mammals have relied on breastfeeding to keep infants alive for thousands of years. Breastfeeding is designed to sustain a baby completely until they start to eat family foods after six months and is then part of the natural diet for at least two to four years of age! Surely it can’t suddenly have become unreliable?
Lets have a look at the known indicators your baby is getting enough milk:
Your baby is heavily wetting at least 5 disposable nappies (6+ cloth nappies) in 24 hours. And they have regular, soft yellow poo.
Your baby’s growth is following their percentile curve on the growth charts for weight, length and head circumference.
Your baby is generally content after most feeds. All babies will cluster feed and have fussy times of day.
You might be surprised that these are generally NOT the signs worried parents report when seeking support to increase their milk supply! Here’s what the more common concerns are:
Your baby is feeding frequently. While 8-12 breastfeeds in 24 hours is typical, some babies will feed as many as 18 times a day! The most likely reason for the difference is varying stomach capacity. Not milk supply.
Your baby’s feeding pattern has changed. All babies go through times of rapid growth and development and adjust their breastfeeding as needed. Breastfeeds can become longer or shorter, closer together or more spaced apart.
Your baby isn’t sleeping long periods. Expectations of infant sleep are very different to the reality. The association between how much a baby sleeps and how much milk they are getting is inaccurate and unreliable.
Your baby is cluster feeding: It is typical for babies to increase the frequency and length of breastfeeds during the late afternoon or early evening. This cluster feeding is also known as The Witching Hour by parents who still have their sense of humour intact!
Your baby doesn’t feed as long: In the early days, babies take a while to feed (even up to an hour!) and often fall asleep at the breast. As they mature, they can quickly remove milk (maybe just five minutes!) and might need other help to settle to sleep after feeds. Around four months, babies become easily distracted and feeds can be short.
Your breasts don’t feel full anymore: Around 6-12 weeks (but sometimes sooner and sometimes later) your breasts change how they make milk and no longer fill up between feeds. Instead, they produce the milk while your baby is drinking it! Your breasts will feel softer and only become firm if you delay or skip a breastfeed.
Your breasts never leak milk and/or you don’t feel a let-down: Every breast is different. Some constantly secrete milk between feeds and need lots of breast pads to soak it up, others never waste a drop of that precious liquid! It all comes down to the ability of tiny little muscles to keep it in! And the sensation of the let-down reflex varies so much between individuals, there is no one-way to describe it. Some mothers even notice a huge difference in their own experiences across several babies. You can usually know a let-down has occurred as your baby will start pausing longer to swallow between sucking.
You can’t express or pump any breastmilk: While some women can express extreme amounts of breastmilk and are able to fill their freezer or donate to other babies, most women can only express around 20-50mls per session and others have breasts that just will not give up their milk to anything other than the baby. This doesn’t indicate how much milk you make or how much milk your baby is getting. If you need to express to return to work or for other regular separations from your baby then getting the right breast pump and pumping routine will help. It is very common not to be able to express large volumes after the 6-12 week change in milk production.
Your baby will drink a whole bottle of formula: drinking from a bottle is a totally different experience for your baby. The flow of breastmilk changes during a feed, gradually slowing and becoming richer with every mouthful. When a baby is given a bottle, they keep on swallowing until the milk is gone, no matter how much you offer! Babies are waiting for the flow to change, which it never does, so they just keep going. Your baby might even be distressed after a large top-up following a breastfeed as their stomach is overstretched and painful. Babies will often vomit up excess milk. Paced feeding allows bottle fed babies to regulate their appetite with slower feeding.
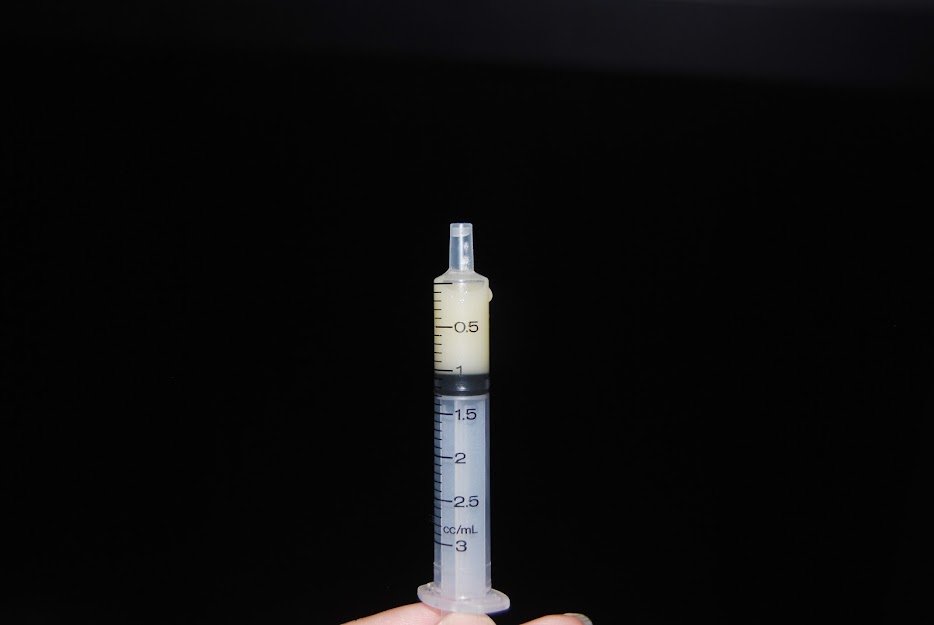
A good pumping session between breastfeeds is around 20 -50mls
Some reasons your milk supply might be low are due to misinformation from advisers:
Routines and schedules can interfere with your milk supply because your baby is not naturally communicating their needs with your breasts. Your body needs feedback from your baby’s natural feeding cycle to make enough milk for their current needs and growth. Put away the charts and training manuals and follow your baby.
Dummies and top-ups can reduce your supply if used to stretch out feeds or make your baby sleep longer. Your breasts need your baby’s sucking to match supply to demand. Comfort sucking is totally normal at the breast and most babies don’t need dummies.
Following a clock to time feeds or the time between feeds is not necessary and can interfere with your milk production. Apps which record this data might seem reassuring but should not be used to restrict babies time at the breast.
One side per feed: Some mothers worry their baby won’t get the fat-rich milk which used to be described as hind-milk. They have been told this milk comes at the end of a feed and they must leave the baby on the first breast to receive it. This misunderstanding of how breasts make milk often leads to babies missing out on a whole breast of milk waiting for them and the breasts reduce production in response to less frequent stimulation. If your baby seems hungry after they come off the first breast and show signs of seeking the breast, offer the second side! They can even come back to the first again to “lick the plate”if they want to! No limits!
Following a sleepy baby’s lead. Most healthy full-term babies will wake and seek the breast every couple of hours. However, there are babies who can’t be relied on to wake often enough. These might seem the baby of your dreams, sleeping long hours and even self-settling sometimes. In fact, these placid little people who don’t make a fuss can be a problem. Frequency of breastfeeds needs to be controlled by the mother if a baby cannot be relied on to wake often enough. Some babies are sleepy due to jaundice in the first weeks. Pre-term babies tend to sleep more and need to be woken to feed. And some are just placid babies who doze back to sleep before feeding cues reach their parents in another part of the house. These babies need to be close to their mother so she can respond quickly. To meet the minimum of 8 feeds in 24 hours, babies shouldn’t sleep longer than 3 hours and might even need waking after two to get sufficient feeds in their day. “Never wake a sleeping baby ” isn’t always a good rule of thumb.
If your supply has dropped due to these practices, you can boost it again by effective and frequent removal of milk.
Some people really can’t exclusively breastfeed
Biologically, the majority of mothers and babies have everything they need to reach their breastfeeding goals. Very rarely there are circumstances which might prevent a baby being fully - or even partially - breastfed. Often pre-existing health conditions are identified before or during pregnancy and the mother is counselled on what to expect.
Breast development begins in puberty and continues during pregnancy. Very rarely, breasts do not develop typically. Some women can have Insufficient Glandular Tissue (IGT) or hypoplasia of the mammary gland. These breasts cannot lactate to fully meet the baby’s needs however partial breastfeeding can be possible and some mothers go on to have a significant breastfeeding relationship with their child despite needing to supplement at all or most feeds.
Previous breast surgery or injury might mean the duct system or nerves are damaged and cannot fully function. Some lactation might occur and babies can be partially breastfed with supplementation. Individual breasts might be differently impacted: if one side can’t function well the other side might.
Chronic health conditions like Polycystic Ovarian Syndrome (PCOS) and hypothyroidism affect hormonal function which can affect milk production. Partial breastfeeding can still be possible.
Significant blood loss during/after childbirth, known as postpartum haemorrhage, can disrupt the natural lactation process. In rare cases, shock impacts the pituitary gland function.
There are just a few medical conditions where mothers are advised not to breastfeed at all. Few medications are contraindicated while breastfeeding. Although many medications do pass into breast milk, most have no known adverse effect on milk supply or on infant well-being.
If your baby needs to be routinely fed donor breastmilk and/or infant formula, a Supplemental Nursing System allows you to do so during breastfeeds.
Some babies cannot exclusively breastfeed
Most babies are born ready to breastfeed. But sometimes exclusive breastfeeding is not possible.
Cleft lip, cleft palate and cleft lip and palate are among the most common congenital deformities and affect 1.1 in 1000 infants. While many infants with a cleft lip only can be directly fed at the breast, those with a cleft palate are usually unable to create the vacuum needed to effectively remove milk from the breast. Babies can be exclusively fed expressed breastmilk, donor milk fed and/or fed infant formula from purpose-designed bottles.
Premature babies born before 32 weeks may not yet have developed the suck reflex and babies born before 36 weeks may have a weak or immature suck. However, sometimes babies aa early as 26 weeks surprise everyone by latching eagerly! However, very premature babies will generally be fed expressed breastmilk via a naso-gastric tube for many months. Oral aversion happens due to unpleasant experiences associated with invasive, but necessary, medical care. Some babies refuse the breast, bottles or other methods of feeding and continue tube feeding long-term. Babies can be exclusively fed expressed breastmilk, donor milk fed and/or fed infant formula.
There are a few rare genetic metabolic conditions that mean fully breastfeeding may not be possible. However, partial breastfeeding in addition to specialised infant formulas might be an option. Conditions include: Galactosemia, Phenylketonuria (PKU) and Maple Syrup Urine Disease.
Primary (or true) lactose intolerance
This extremely rare genetic condition is present from birth and is life-threatening. Babies fail to thrive and need a special diet. This is NOT the same as Secondary Lactose Intolerance which is temporary and can be resolved once the cause is identified and the gut is able to heal.
How can your prevent low supply?
The majority of breasts are capable of meeting a baby’s full nutritional needs in the first six months of life and continue to be a significant part of their diet into the third year and beyond.
Frequent removal of colostrum in the hours and days after birth has an important role in establishing milk production. If a baby cannot go to the breast immediately, a mother should be supported to have colostrum hand expressed within the first hour after birth. Expressing should continue at least every three hours, day and night, until the baby is effectively removing milk at the breast themselves. The volume of colostrum will be small -0.5ml - 1.00ml is typical. It is the removal, not the amount, which is important. This signals the breast to activate milk production
Achievement!